- Review
- Open access
- Published:
Convergence of tissue engineering and sustainable development goals
Biotechnology for Sustainable Materials volume 1, Article number: 20 (2024)
Abstract
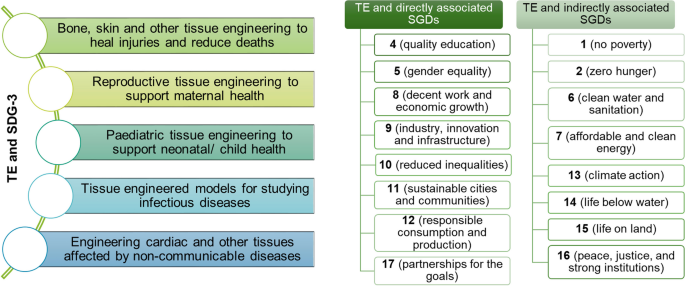
The convergence of sustainability with medical innovation in tissue engineering represents a pivotal advancement in both biomedical science and environmental stewardship. This review article provides a comprehensive overview of how tissue engineering integrates sustainable practices while advancing medical treatments. It delves into the core components of tissue engineering, focusing on the development and application of biomaterials such as polymers, metals, ceramics, composites, and decellularized materials. The article also explores cutting-edge technologies like bioprinting, electrospinning, cell sheet engineering, and microfluidics, highlighting their contributions to creating effective and eco-friendly medical solutions. A significant portion of the review is dedicated to sustainability and the Sustainable Development Goals (SDGs), with a particular emphasis on SDG 3 (Good Health and Well-being) and its intersection with tissue engineering. The covers other relevant SDGs, demonstrating how sustainable biomaterials and technologies contribute to broader objectives such as SDG 4, 5, 8, 9, 10, 11, 12, 17. Additionally, the discussion extends to other indirectly relevant SDGs such as SDG 1, 2, 6, 7, 13, 14, 15, 16. The article concludes with a summary of current advancements and prospects, emphasizing the importance of integrating eco-conscious approaches in tissue engineering to achieve a sustainable and innovative medical future.
Graphical Abstract
Introduction
The Sustainable Development Goals (SDGs) act as a global framework for achieving a more inclusive, equitable, and sustainable future [1]. Tissue engineering domain which emerged in the late 1980s, to create living, functional tissues in the laboratory for implantation in patients, thereby advancing regenerative medicine and personalized healthcare solutions [2]. Initially conceptualized to match the mechanical properties of native tissues and minimize harmful host responses, tissue engineering has significantly evolved, focusing now on creating constructs that not only integrate seamlessly with the body but also support functional restoration through biological compatibility and sustainability. The advent of tissue engineering has coincided with a growing global emphasis on sustainability, aligning with the SDGs established by the United Nations. The integration of sustainable practices in tissue engineering involves the use of eco-friendly materials in scaffold fabrication, green manufacturing processes, and the development of biodegradable and biocompatible biomaterials. These efforts underscore the importance of innovative research, collaborative partnerships, and regulatory support in advancing both the field of tissue engineering and global sustainability goals.
The review starts with an overview of tissue engineering, which includes an introduction, key aspects, and applications of tissue engineering. Following this, the review describe an overview of biomaterials, trends in biomaterials and the critical role of biomaterials in tissue engineering. Then, the review outlines the sustainable technologies involved in tissue engineering, by explaining the two different approaches of tissue engineering, the critical role of scaffolds in tissue engineering, and technological trends in tissue engineering. Then, the review discusses sustainability and SDGs as per the United Nation’s 2030 Agenda for Sustainable Development. It further provides deeper insights into sustainability in different fields like health care, biomedical engineering, and tissue engineering. Subsequently, this review explores how different biomaterials and tissue engineering technologies address sustainability issues. The review also analyses the biomaterials and tissue engineering technologies that follow 17 sustainable development guidelines. Finally, the review ends a summary and future perspectives. This review attempts to integrate how various aspects of biomaterials and innovative technologies within the field of tissue engineering align with sustainable development goals, particularly SDG 3, and thus highlight the convergence of sustainability with medical innovation.
Tissue engineering
Introduction to tissue engineering
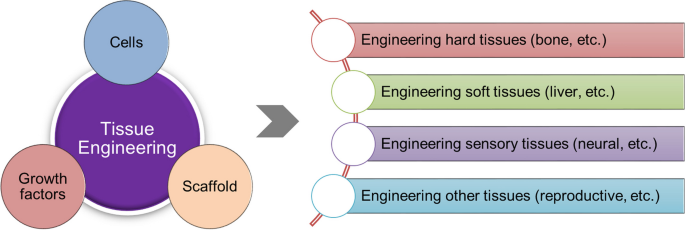
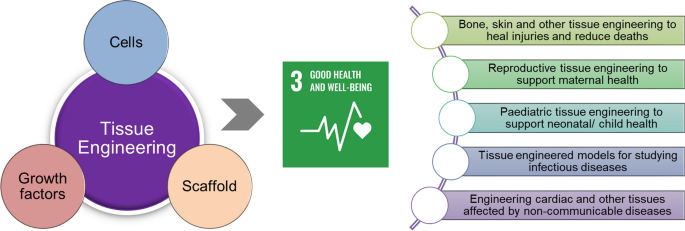
Tissue engineering is an interdisciplinary field that combines the concepts of life sciences, engineering, and medicine to develop biological substitutes capable of repairing, maintaining, or improving tissue function (Fig. 1). This field aims to create living, functional tissues in the laboratory that can be implanted into patients to restore normal function or facilitate healing, thus offering significant potential for advancing regenerative medicine and personalized healthcare solutions [2]. Tissue engineering was first introduced in the late 1980s in a meeting held by the National Science Foundation in the USA [3], while the paper entitled “Functional Organ Replacement: The New Technology of Tissue Engineering” in the year 1991 was first to use the term tissue engineering as it is known presently [4]. Tissue engineering can be achieved through ex vivo or in situ strategies, each with its own set of challenges and opportunities. Ex vivo strategies involve engineering tissue constructs in the lab before implantation, while in situ strategies involve delivering cells and/or a bioscaffold directly to the defect site to stimulate tissue repair [5]. As an industry, tissue engineering has experienced significant growth and reasonable commercial success in recent years [6]. Classically, tissue engineering recapitulates tissue and organ formation in our body to varying degrees, bringing together cells in a three-dimensional (3D) fabricated environment where appropriate signals are provided for tissue formation. In parallel, the evolution of tissue engineering research is intertwined with progress in other fields through the examination of cell function and behavior in isolated biomimetic microenvironments [7]. tissue engineering applications now extend beyond regeneration strategies alone, operating as a platform for modifiable, physiologically representative in vitro models [8].
Key aspects of tissue engineering
TE requires a triad of components: (1) Harvested and dissociated cells from the donor tissue; (2) scaffolds made of biomaterials on which cells are attached and cultured, then implanted at the desired site in functioning tissue; and (3) growth factors that promote and/or prevent cell adhesion, proliferation, migration, and differentiation by up-regulating or down-regulating the synthesis of protein, growth factors, and receptors. A relevant selection of cells, a biomaterial scaffold, and the presence of appropriate signals coordinate to ultimately recreate tissue to address the limitations of current treatments for tissue and organ damage, such as donor shortages and rejection issues. The interaction between the tissue engineering triad is necessary to optimize the development of tissue in vitro [2]. These scaffolds can be fabricated from various materials, including biodegradable polymers, which degrade over time to allow for tissue integration and remodeling. The architecture of scaffolds, including their porosity and mechanical properties, was tailored to match the requirements of specific tissues, influencing cell behavior and subsequent tissue formation [9]. Cells used in tissue engineering can be derived from different sources, including embryonic stem cells, bone marrow-derived mesenchymal stem cells (MSCs), and cord-derived MSCs. These cells are capable of differentiating into various cell types, making them suitable for regenerating a wide range of tissues. The choice of cell type depends on the target tissue and the specific requirements for regeneration. Signalling molecules, including growth factors and cytokines, play a pivotal role in regulating cellular activities such as proliferation, migration, and differentiation. These molecules can be incorporated into the scaffolds to provide localized and sustained delivery, enhancing the regenerative potential of the engineered tissue. The controlled release of these signalling molecules from the scaffold ensures that cells receive the necessary cues for appropriate tissue development. Together these three components form the foundation of tissue engineering strategies aimed at restoring, maintaining, or improving tissue function [10].
Applications of tissue engineering
Tissue engineering has catered to create constructs that can effectively replace or support the functions of native tissues. The applications help in the regeneration of skin, bone, cardiac, liver, and nerve tissues. Skin tissue engineering was one of the most advanced areas, focusing on creating grafts for burn victims and patients with chronic wounds. Engineered skin constructs like Apligraf® and Dermagraft® are already in clinical use [11]. Additionally, advancements in 3D bioprinting allow for the precise deposition of cells and biomaterials to create layered skin structures that mimic the complexity of natural skin [12]. Bone tissue engineering aims to address issues such as fractures, osteoporosis, and bone defects. Techniques involve the use of biocompatible scaffolds made from materials like hydroxyapatite, tricalcium phosphate, and bioactive glasses, which provide structural support and promote osteogenesis [13]. Stem cells, particularly MSCs, are commonly used to differentiate into osteoblasts. The scaffolds are often enhanced with growth factors like bone morphogenic protein-2 to stimulate bone growth [14]. Cardiac tissue engineering addresses heart diseases and myocardial infarction by developing constructs that can repair or replace damaged heart tissue. Techniques such as patch grafts, where engineered cardiac tissue was applied to the infarcted area, have shown promise in improving heart function [15]. Biomaterials including natural polymers like fibrin and synthetic polymers like poly (glycerol sebacate) were explored in cardiac tissue engineering. Additionally, electrical stimulation was often used to enhance the maturation and functionality of the engineered cardiac tissue [16]. Liver tissue engineering seeks to develop functional liver tissues for transplantation and in vitro models for drug testing. Techniques involve the use of hepatocytes or stem cells seeded onto scaffolds. The goal was to create constructs that can perform essential liver functions. Advances include bioprinting liver tissues with precise architecture and incorporating vascular networks to support cell viability and function [17]. Nerve tissue engineering aims to repair peripheral nerve injuries and spinal cord damage. Techniques involve the use of scaffolds designed to guide axonal growth and support neural cell adhesion. Biomaterials such as poly (lactic-co-glycolic acid) (PLGA) and chitosan are commonly used, often combined with neurotrophic factors like nerve growth factor to promote nerve regeneration. Stem cells, including neural stem cells and MSCs, are also utilized for their potential to differentiate into neurons and glial cells. Clinical applications include the development of nerve conduits for bridging nerve gaps and enhancing functional recovery [18]. Tissue engineering also encompasses diverse applications such as corneal regeneration [19], ear cartilage engineering [20], and laryngeal tissue development [21], while dental pulp regeneration provides treatments for tooth decay and injury [22]. These examples demonstrate the broad scope and transformative potential of tissue engineering in medical interventions.
Biomaterials in tissue engineering
Introduction to biomaterials
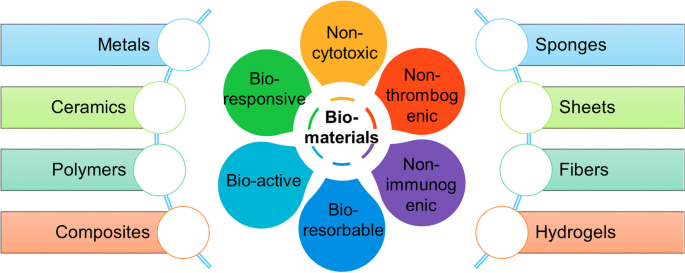
Biomaterials play a crucial role in tissue engineering, a field that combines engineering and biology to develop methods for replacing or regenerating human tissues. They are designed to provide an architectural framework reminiscent of native extracellular matrix (ECM) to encourage cell growth and eventual tissue regeneration [23]. An important avenue of tissue engineering is the development of biomaterials that can promote regenerative processes by effectively transporting cell populations and therapeutic agents, as well as providing structural scaffolding that confers sufficient mechanical properties to tissues. Moreover, the degradation rate of the biomaterial should ideally match the rate of new tissue formation at the implantation site, ensuring that the scaffold supports the regenerating tissue without leaving gaps or degrading prematurely [24]. Biomaterials have a long history of use in medical applications, such as intraocular lenses and dental fillings, but advances in cell and molecular biology, chemistry, materials science, and engineering have expanded their potential uses in clinical settings. Over the past 50 years, the definition of the ideal biomaterial has evolved significantly (Fig. 2). Initially, biomaterials were designed to be inert, matching the mechanical properties of native tissues and avoiding harmful host responses [25]. Early materials included bone cement, stainless steel, and Dacron, which were chosen for their mechanical properties and predictable foreign body responses. However, second-generation biomaterials, such as titanium, bioglass, PLGA, and collagen, were developed with bioactive properties like osseointegration, tissue integration, and biodegradation [26]. Hydrogels have been preferred for biomedical applications due to their excellent biocompatibility, adaptable structures, versatile synthesis methods, and favorable physical properties [27, 28].
A wide range of biopolymers are being used to replace synthetic polymers across various industries, including biomedical [29]. Additionally, there are bio-based polymeric materials, like proteins, polysaccharides, and aliphatic polyesters, that are derived from plants, animals, or microbial synthesis, and offer eco-friendly approaches to enhancing sustainability [30]. These polymers differ from other biopolymers and can be either biodegradable or non-biodegradable [31]. Materials derived from biomass have minimal carbon footprints and possess multifunctional properties essential for promoting sustainability [32]. One such biomaterial was bacterial cellulose, which has been suggested for use in various biological applications, including wound healing, the production of artificial blood vessels, soft tissue engineering, and bone tissue engineering [33].
Trends in biomaterials
Currently, the focus is on biomaterials that integrate with adjacent tissues and enhance regenerative or reconstructive capacities. These materials are bioinductive, promoting the body's natural healing processes rather than merely being inert placeholders. The ECM is nature's template for biomaterials, providing support and scaffolding for cell growth. Scaffold materials in tissue engineering can be synthetic or naturally occurring [25]. Regardless of origin, they must support cell attachment, maintenance, proliferation, and sometimes differentiation while providing adequate structural support for the intended site. Additionally, the host response to these materials was critical for long-term success, especially in pediatric patients, where the scaffold must adapt to the growth and development of surrounding tissues [25]. Recent advancements in biomaterials for tissue engineering include the development of smart biomaterials that respond to external stimuli such as temperature, pH, magnetic, or electric fields. These materials offer dynamic properties that can better mimic natural tissue behavior. For instance, 3D and 4D bioprinting technologies have enabled the creation of complex, tissue-like structures that can change over time in response to environmental changes [34]. The clinical translation of tissue engineering strategies relies heavily on advancements in biomaterial development. While the application of these materials in pediatric patients remains limited, ongoing research aims to improve our understanding of the molecular environment during tissue regeneration, ultimately enhancing the effectiveness of tissue engineering approaches [25].
Critical role of biomaterials in tissue engineering
Biomaterials, that make scaffolds, play a critical role in tissue engineering, providing a platform for cell attachment and growth; therefore, the influence of scaffold characteristics on cell behavior is a key area of study [35]. Scaffolds direct the growth of cells seeded within the porous structure of the scaffold. Biomaterials significantly influence the fate of tissue engineering through their surface chemistry, mechanical properties, degradation profiles, and ability to deliver bioactive molecules [36]. Surface chemistry is critical as it affects protein adsorption, cell adhesion, and subsequent cell behavior. For instance, materials with specific cell-binding domains such as RGD (arginine-glycine-aspartic acid) can enhance cell adhesion, which is essential for tissue regeneration. Additionally, the surface modification of biomaterials with bioactive molecules like peptides and growth factors can further promote cell proliferation, migration, and differentiation [37]. The degradation rate of biomaterials is another vital aspect that influences tissue regeneration. An optimal degradation rate ensures that the scaffold provides adequate support for new tissue formation but degrades at a pace that does not impede the reconstruction process. Incorporating enzyme-sensitive peptides into biomaterials can control degradation rates, facilitating a balance between scaffold support and degradation [38].
Mechanical properties such as stiffness and elasticity also play a crucial role. They must match the native tissue's properties to support cell growth and tissue formation. For example, materials engineered for bone tissue engineering often include components like hydroxyapatite to provide the necessary mechanical strength [34]. The mechanical environment can influence cellular processes, including stem cell differentiation and tissue morphogenesis. Surface topology, including micro- and nanoscale patterning, can direct cellular responses even in the absence of biochemical signals [36]. Studies have shown that features such as particle shape and surface roughness can affect cell adhesion, proliferation, and differentiation. For instance, specific topographical cues can induce stem cells to differentiate into particular lineages, aiding in the development of functional tissues. Furthermore, the delivery of bioactive molecules through biomaterials is essential for guiding tissue regeneration [39]. Growth factors and peptides can be coupled with scaffolds to promote specific cellular activities. For example, biomaterials can be designed to release growth factors in a controlled manner to enhance angiogenesis and osteogenesis, vital for the regeneration of complex tissues such as bone and cartilage. The integration of biomaterials with the ECM components is also crucial. The ECM provides structural and biochemical support to surrounding cells, influencing cell behavior and tissue development. Biomaterials mimicking the ECM's properties can facilitate better integration with host tissues, promoting more effective tissue regeneration [40]. When a scaffold is implanted into the affected area, it should provide structural support for cell adhesion, proliferation, migration, and differentiation, promoting cellular activity similar to the in vivo environment. Additionally, it should allow for the controlled release of growth factors to regulate cell proliferation, viability, and differentiation [41].
Technologies in tissue engineering
Introduction to tissue engineering approaches
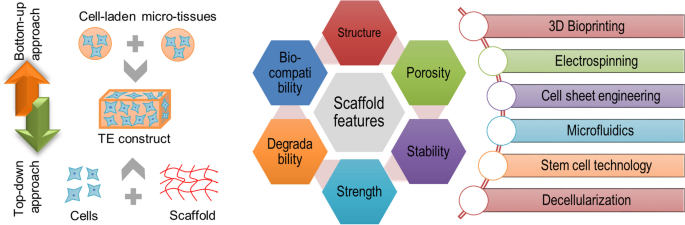
Tissue engineering involves the fabrication of tissue constructs either in a bottom-up or top-down approach (Fig. 3). In the bottom-up approach, small building blocks such as cells, micro-tissues, or scaffolding materials are assembled to create more complex structures. This method focuses on the self-organization and self-assembly properties of cells and biomaterials, allowing for the precise design and fabrication of tissue constructs from the molecular or cellular level. Techniques like 3D bioprinting, layer-by-layer assembly, and the use of cell-laden hydrogels are common in bottom-up tissue engineering [42]. These techniques enable the creation of highly detailed and customizable tissue structures by placing cells and materials exactly where needed to mimic the natural architecture of tissues. 3D bioprinting, for example, involves the deposition of cell-laden bio-inks layer by layer to build complex tissue constructs. This technique allows for high precision and control over the placement of different cell types and materials, facilitating the creation of heterogeneous and functional tissues. The bottom-up approach also includes methods like organoid culture, where stem cells are guided to form miniaturized and simplified versions of organs, which can be used for disease modeling, drug testing, and regenerative medicine [43].
In contrast, the top-down approach starts with a pre-existing bulk material or scaffold, which is then shaped and modified to achieve the desired tissue structure. Techniques like electrospinning, freeze-drying, and molding are commonly used to create scaffolds with specific shapes and properties that support cell attachment, proliferation, and differentiation. Electrospinning, for instance, produces nanofibrous scaffolds that mimic the fibrous structure of natural ECM, providing a conducive environment for cell growth and tissue regeneration [44]. Freeze-drying can create porous scaffolds with high surface area, enhancing nutrient diffusion and cell infiltration. These top-down techniques leverage the inherent advantages of pre-existing materials and structures to guide tissue formation, often resulting in constructs that closely resemble the native tissue in terms of architecture and mechanical properties [45]. This approach also involves the use of decellularized tissues or organs, which retain the natural ECM architecture and mechanical properties of the original tissue [46]. The decellularized scaffold is then repopulated with patient-specific cells to regenerate functional tissues.
Both the bottom-up and the top-down methods have their unique advantages and challenges. The bottom-up approach allows for greater control over the microarchitecture and composition of the tissue, making it suitable for creating complex and heterogeneous structures. However, it can be limited by the difficulty in scaling up to larger tissue constructs. The top-down approach benefits from the use of natural scaffolds with inherent biological cues, but it may face challenges in achieving precise control over the microenvironment and integrating different cell types and materials.
Critical role of scaffold in tissue engineering
Scaffolds in tissue engineering are essential for directing cell behavior, tissue formation, and integration with host tissues. Their properties, such as porosity, mechanical strength, degradation rate, and surface characteristics, significantly influence the overall fate of the engineered tissue. Porosity is a key scaffold property that affects cell infiltration, nutrient diffusion, and waste removal [47]. Highly porous scaffolds provide ample space for cells to migrate and proliferate, which is essential for tissue regeneration. The size and interconnectedness of pores are crucial for vascularization, which supplies the engineered tissue with oxygen and nutrients. Optimal pore sizes vary depending on the type of tissue being engineered. For example, larger pores are typically beneficial for bone tissue engineering, while smaller pores are better suited for skin or cartilage regeneration. Mechanical strength and stiffness of the scaffold are also vital; scaffolds must mimic the mechanical properties of the target tissue to provide appropriate cues for cell differentiation For instance, softer scaffolds are preferred for neural or adipose tissues, whereas stiffer scaffolds are necessary for bone or cartilage tissues [48]. The mechanical properties influence mechano-transduction, where cells convert mechanical stimuli into biochemical signals, affecting gene expression and cell behavior. This property ensures that cells experience a similar environment to their native tissue, promoting proper tissue formation and function [49].
The degradation rate of the scaffold must be carefully controlled to match the rate of new tissue formation. A scaffold that degrades too quickly may not provide sufficient support for cells, while one that degrades too slowly can impede tissue integration and function. Biodegradable materials like polylactic acid (PLA) and polyglycolic acid are commonly used for their ability to break down into non-toxic byproducts, which are then absorbed or excreted by the body. The degradation products should not induce inflammation or toxicity, ensuring a safe environment for tissue regeneration [50]. Surface characteristics, including topography and chemical functionality, play a significant role in cell adhesion, proliferation, and differentiation. Surface modifications, such as coating with ECM proteins (e.g., collagen, fibronectin) or incorporating bioactive molecules (e.g., growth factors), can enhance cell-scaffold interactions [51]. Nanoscale features on the scaffold surface can mimic the natural ECM, providing cues that promote cell attachment and growth. Techniques like electrospinning can create nanofibrous scaffolds that replicate the fibrous nature of native tissues, supporting cellular behavior and tissue development [52].
Nanoscale scaffolds offer a higher surface area-to-volume ratio compared to microscale scaffolds, which can enhance cell adhesion and proliferation. Nanoscale features provide more precise topographical cues that mimic the natural ECM, promoting more natural cellular behaviours. Microscale scaffolds, however, can better facilitate cell infiltration and nutrient diffusion, which is crucial for the survival and function of larger tissue constructs. These scaffolds often support the formation of more substantial tissue masses and can be designed to include macroscopic features that aid in vascularization, a critical aspect of the viability of engineered tissues [53]. The interplay between these scaffold properties ultimately determines the success of the tissue engineering endeavour. By carefully designing and optimizing scaffold characteristics, researchers can create environments that closely mimic natural tissues, guiding cells toward the desired outcomes. This approach not only enhances the functional integration of engineered tissues but also improves the clinical applicability and success rates of tissue engineering therapies [54].
Technological trends in tissue engineering
Tissue engineering employs a variety of technologies to create functional tissues and organs, each with distinct methodologies and applications. One key technology is 3D bioprinting, which utilizes layer-by-layer deposition of bio-inks containing cells and biomaterials to fabricate complex tissue constructs. This technique allows for precise placement of cells and ECM components, enabling the creation of tissues with intricate architectures. For example, researchers have used 3D bioprinting to create skin grafts, cartilage, and vascularized tissues, demonstrating its potential for personalized medicine and complex tissue reconstruction [55]. Electrospinning is a technique used to produce nanofibrous scaffolds that mimic the fibrous structure of a natural ECM. These scaffolds provide a conducive environment for cell attachment, proliferation, and differentiation, making them suitable for applications in wound healing, nerve regeneration, and vascular grafts. Electrospun scaffolds have been successfully used to create artificial blood vessels and support the regeneration of peripheral nerves [56].
Microfluidics technology involves the manipulation of fluids at the microscale to create controlled microenvironments for cell culture and tissue engineering. Microfluidic devices can mimic the physiological conditions of tissues, allowing for the study of cell behaviors, drug testing, and the creation of tissue models. For instance, microfluidic chips have been used to create liver-on-a-chip models for drug toxicity testing and to develop vascularized tissue constructs for studying angiogenesis [57]. Organoid culture is a technology that uses stem cells to create miniaturized and simplified versions of organs in vitro. These organoids can recapitulate key aspects of organ development, function, and disease, providing valuable models for basic research, drug discovery, and regenerative medicine. Organoids have been developed for various tissues, including the brain, intestine, kidney, and liver, offering insights into tissue-specific physiology and pathology [58].
Stem cell technology is fundamental to tissue engineering, as it provides a source of cells capable of differentiating into various tissue types. Induced pluripotent stem cells and embryonic stem cells can be directed to form specific cell types and tissues, enabling the creation of patient-specific tissue constructs. Stem cell-derived tissues have been explored for applications in cardiac repair, spinal cord injury, and diabetes treatment [59]. Another important technology is decellularization, which involves removing cellular components from donor tissues or organs, leaving behind a scaffold composed of ECM. This scaffold retains native tissue architecture and mechanical properties, making it an ideal template for recellularization with patient-specific cells. Decellularized scaffolds have been used to engineer heart valves, lungs, and liver tissues, offering promising solutions for organ transplantation without the risk of immune rejection [60].
These technologies highlight innovative solutions for tissue repair and regeneration. The continuous advancement in these technologies holds promise for addressing the growing need for functional tissues and organs in regenerative medicine and transplantation.
Sustainability and sustainable development goals
Introduction to sustainability and sustainable development goals
Sustainability is defined as development that meets the needs of the present without compromising the ability of future generations to meet their own needs. Adopted by all United Nations Member States in 2015 as part of the 2030 Agenda for Sustainable Development, the SDGs build on decades of work by countries and the UN, including the Millennium Development Goals. SDGs are a collection of 17 interlinked global goals designed to achieve a better and more sustainable future for all. The SDGs cover a broad range of social, economic, and environmental development issues and aim to address the global challenges we face, including poverty, inequality, climate change, environmental degradation, peace, and justice. They are unique in that they call for action by all countries, developed and developing, to promote prosperity while protecting the planet. Technically, the SDGs are grounded in a comprehensive set of 169 specific targets that are measurable and time-bound. Each goal has specific targets to be achieved over the next 15 years. The targets are designed to be monitored through a set of indicators developed by the Inter-Agency and Expert Group on SDG Indicators. A key feature of the SDGs is their universality. Technological innovation and digital transformation also play critical roles in advancing the SDGs. Partnerships and collaboration among governments, the private sector, civil society, and international organizations are crucial for the success of the SDGs. The goals explicitly acknowledge the need for multi-stakeholder partnerships to mobilize and share knowledge, expertise, technology, and financial resources.
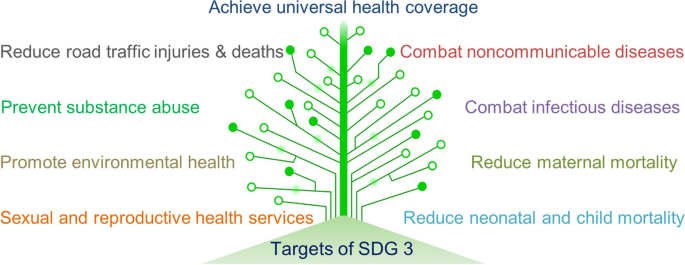
Sustainability in healthcare
Healthcare is primarily addressed in SDG-3 "Ensure healthy lives and promote well-being for all at all ages". This goal encompasses a wide range of targets aimed at improving health outcomes, reducing mortality rates, and addressing global health challenges. SDG-3 includes 9 targets (Fig. 4) which aim to: (3.1) reduce the global maternal mortality ratio to less than 70 per 100,000 live births; (3.2) end preventable deaths of newborns and children under 5 years of age; (3.3) end the epidemics of AIDS, tuberculosis, malaria, and neglected tropical diseases, and combat hepatitis, water-borne diseases, and other communicable diseases; (3.4) reduce by one-third premature mortality from non-communicable diseases (NCDs); (3.5) strengthen the prevention and treatment of substance abuse; (3.6) halve the number of global deaths and injuries from road traffic accidents; (3.7) ensure universal access to sexual and reproductive health-care services, and the integration of reproductive health into national strategies and programs; (3.8) achieve universal health coverage, access to quality essential health-care services, and access to safe, effective, quality, and affordable essential medicines and vaccines for all; (3.9) substantially reduce the number of deaths and illnesses from hazardous chemicals and air, water, and soil pollution and contamination; and other means of implementation for the targets viz. (3a) strengthen the implementation of the World Health Organization Framework Convention on Tobacco Control in all countries, as appropriate; (3b) support the research and development of vaccines and medicines for the communicable and NCDs that primarily affect developing countries, provide access to affordable essential medicines and vaccines, and ensure that intellectual property rights do not undermine this goal, in line with the Doha Declaration; (3c) substantially increase health financing and the recruitment, development, training, and retention of the health workforce in developing countries, especially in least developed countries and small island developing states; and (3d) strengthen the capacity of all countries, particularly developing countries, for early warning, risk reduction, and management of national and global health risks.
Sustainability in biomedical engineering
Biomedical engineering drives the creation of cutting-edge healthcare infrastructure, including advanced medical facilities equipped with state-of-the-art technology. These innovations not only improve patient outcomes but also stimulate economic growth through the development of a robust biomedical industry. Apart from contributing to SDG 3, the advancement of biomedical technologies also contributes to SDG 9, which focuses on building resilient infrastructure, promoting inclusive and sustainable industrialization, and fostering innovation. Biomedical engineering also intersects with SDG 12, which advocates for responsible consumption and production. And, the implementation of circular economy principles, where medical devices are designed for durability, reuse, and recyclability, also aligns with SDG 12. Sustainable design and manufacturing practices in the development of medical devices are crucial in minimizing environmental impact. Utilizing biodegradable materials for implants and reducing the use of hazardous substances in medical equipment production are steps toward achieving this goal. SDG 4, which focuses on quality education, is also relevant to biomedical engineering. Providing education and training in biomedical engineering not only equips individuals with the skills needed to innovate in the healthcare sector but also fosters a knowledgeable workforce capable of addressing complex health challenges. Finally, the pursuit of SDG 17, which emphasizes strengthening the means of implementation and revitalizing the global partnership for sustainable development, is essential in biomedical engineering. For example, public–private partnerships in biomedical research and development can lead to the creation of affordable healthcare solutions tailored to the needs of developing countries, addressing disparities in healthcare access and quality.
Sustainability in tissue engineering
Biomaterials such as polymers, metals, ceramics, composites, and decellularized materials, coupled with cutting-edge technologies like bioprinting, electrospinning, decellularization, cell sheet engineering, and microfluidics, are pivotal in advancing the SDGs. The innovations in biomaterials and tissue engineering technologies drive transformative changes across healthcare, environmental sustainability, and economic growth. By enabling precise tissue engineering, sustainable resource management, and enhanced medical treatments, biomaterials and associated technologies contribute significantly to global efforts aimed at achieving sustainable development and improving quality of life worldwide (Fig. 5).
SDG-3 in tissue engineering
Biomaterials and tissue engineering have immense potential to transform healthcare and medical treatment, and therefore, contribute significantly towards SDG 3. For instance, a key target of SDG 3, is maternal mortality, which aims to reduce the global maternal mortality ratio to less than 70 per 100,000 live births by 2030. Various tissue engineering methods and biomaterials are being developed to support maternal health and reduce mortality, which also comes under target 1 of SDG 3. For instance, innovative biomimetic materials can be employed to create placenta-on-a-chip devices that simulate placental function, allowing for detailed pharmacokinetic studies and a better understanding of drug impacts during pregnancy [61]. Additionally, advancements in silk-based biomaterials have shown promise in treating cervical insufficiency, a condition that can lead to preterm birth and increased maternal mortality. These biomaterials, particularly hydrogel systems like alginate, collagen, and fibrin, provide a minimally invasive method to reinforce the cervix, reducing the risk of premature delivery. Biomaterials are being used to develop in vitro models that replicate the female reproductive system, providing crucial insights into conditions like preterm birth, which significantly contributes to maternal mortality [62]. These models allow researchers to study the physiological and pathological states of reproductive tissues under controlled conditions. Additionally, new hydrogel technologies are being investigated to address postpartum hemorrhage, a leading cause of maternal death. These hydrogels can be applied directly to bleeding sites to promote clotting and reduce blood loss effectively. Efforts to integrate biomaterials in clinical applications are further supported by a dedicated funding stream for women's health bioengineering, emphasizing the importance of targeted research and development in this field [63].
Advancements in biomaterials and tissue engineering hold significant promise for achieving SDG 3, specifically Target 2, which aims to end preventable deaths of newborns and children under five. In pediatric tissue engineering, biomaterial scaffolds have been developed to create functional environments conducive to tissue growth and repair. These scaffolds are crucial for neonatal and pediatric applications due to their ability to support cell growth, deliver drugs, and integrate with the host's biological systems, thereby reducing the risk of mortality in young patients. The field of tissue engineering has seen remarkable progress in managing congenital heart diseases, a leading cause of neonatal mortality [64]. Traditional treatments using synthetic grafts face challenges like thrombosis, infection, and limited growth potential. Tissue-engineered solutions, such as biodegradable scaffolds for vascular grafts, heart patches, and valves, offer a promising alternative. These scaffolds can grow and remodel within the patient, providing long-term solutions that adapt to the changing physiology of growing children [64].
The integration of biomaterials and tissue engineering methods offers promising strategies to combat infectious diseases, enhance therapeutic outcomes, and support the regeneration of damaged tissues, thus aligning with the goals of SDG 3, target 3. Engineered biomaterials play a crucial role in enhancing vaccine efficacy by stabilizing antigens, organizing antigen presentation, recruiting antigen-presenting cells, and delivering antigens to lymph nodes, thereby supporting and boosting effective immune responses. For instance, mesoporous silica rods have been developed for in situ modulation of host immune cells, showcasing their potential to create effective vaccines against infectious diseases [65]. Hydrogels, particularly injectable hydrogels, provide a versatile platform for delivering a wide variety of therapeutics due to their high biocompatibility, tunable physicochemical properties, and controlled release profiles. Moreover, biomaterials can be engineered to provide local immunomodulation, which is critical in managing infections by controlling immune responses and preventing tissue damage. Tissue engineering also contributes significantly to SDG 3 by promoting the regeneration of tissues damaged by infections [66].
Biomaterials and tissue engineering provide innovative solutions for treating and managing NCDs, such as cardiovascular diseases, diabetes, and musculoskeletal disorders, as part of SDG-3, target 4. For example, tissue-engineered vascular grafts and cardiac patches are being developed to repair damaged heart tissues and blood vessels, significantly improving the survival rates and quality of life for patients with cardiovascular diseases [67]. These advanced therapies offer regenerative solutions that traditional treatments cannot provide, addressing the root causes of tissue damage and promoting long-term health benefits. The development of biocompatible and biodegradable biomaterials enhances the effectiveness of medical implants and devices used in treating NCDs. For instance, bioresorbable stents made from materials like PLA are designed to dissolve after fulfilling their purpose, reducing complications associated with permanent implants [68]. Additionally, by using patient-specific cells and biomaterials, scientists can engineer tissues and organs tailored to the individual’s unique biological profile. This personalized approach enhances the effectiveness of treatments, reduces the likelihood of rejection, and accelerates recovery times [69].
Tissue engineering technology is being adopted to restore reproductive functions affected by disorders such as infertility and sexual dysfunction. Biomaterial-based drug delivery systems are being designed to provide controlled and sustained release of contraceptives, enhancing their effectiveness and convenience. Biomaterials like alginate, collagen, and hyaluronic acid are being extensively used in facilitating in vitro follicle culture systems that restore fertility for female patient’s post-cancer treatments [70]. Advanced biomedical engineering technologies, including microfluidic chips and 3D printing, have been developed to address reproductive health challenges. These technologies offer precise control over the reproductive microenvironment, improving outcomes in assisted reproductive technology and contraception [71]. Biomaterial-based scaffolds and implants are designed to provide structural support and promote the regeneration of pelvic floor tissues, offering minimally invasive treatment options that improve health outcomes and recovery times [72]. This integration aligns with the goals of SDG 3, Target 7, promoting well-being and healthy lives for all ages.
Biomaterials and tissue engineering technologies could also contribute to other targets of SDG3. For instance, tissue-engineered skin grafts and bone scaffolds can significantly improve recovery outcomes for accident victims by promoting faster and more effective healing of severe wounds and fractures [73]. These technologies enhance trauma care and reduce the long-term impact of injuries, and thus contribute towards target 6 of SDG-3. The development of cost-effective biomaterials and scalable tissue engineering technologies can make advanced medical treatments more accessible and affordable. These innovations contribute to achieving universal health coverage by providing high-quality, affordable medical solutions, part of target 8 of SDG-3. Tissue-engineered models of the liver and lungs can be used to study the toxicological impacts of pollutants and develop strategies to reduce exposure and harm [74]. These models enable more accurate assessments of how pollutants affect human tissues, leading to better regulatory policies and protective measures; and thus, contribute towards target 9 of SDG-3. An indicative list of how tissue engineering aligns with specific targets under SDG 3 (Good Health and Well-being) is presented in Table 1.
Associated SDGs in tissue engineering
Biomaterials and technologies in tissue engineering are intricately linked with several other SDGs. For instance, tissue engineering contributes to SDG 4 (Quality Education) by enhancing educational experiences through innovative learning tools like bioprinted tissues and organ models, providing hands-on experience and a deeper understanding of human anatomy and disease mechanisms [77]. Promoting gender equality (SDG 5) in tissue engineering involves initiatives like targeted scholarships, mentorship programs, and inclusive policies to support women's participation and professional growth in STEM fields. Towards SDG 8 (Decent Work and Economic Growth), the tissue engineering sector drives economic growth and job creation across biotechnology, pharmaceuticals, and healthcare, with various companies generating high-skilled employment opportunities [6]. As part of SDG 9 (Industry, Innovation, and Infrastructure), tissue engineering fosters industry innovation through advanced technologies like 3D bioprinting, electrospinning, and microfluidics, and establishes robust research infrastructure via partnerships between academia, private companies, and government agencies [78].
Besides, developing cost-effective biomaterials and scalable technologies ensures that advanced medical treatments are accessible in low- and middle-income countries, reducing health disparities and promoting equitable healthcare; therefore, contributing towards SDG 10 (Reduced Inequality). As part of SDG 11 (Sustainable Cities and Communities), minimizing medical waste by using biodegradable biomaterials, using bioprinting technologies to mass produce tissues for highly demanding urban populations, integration of smart technologies contributes to the development of sustainable healthcare system in urban settings [79]. Further, the use of renewable and biodegradable materials in tissue engineering, such as silk fibroin from seri-farming, reduces environmental impact and aligns with SDG 12 (Responsible Consumption and Production) [80]. Last but not least, achieving SDGs through tissue engineering relies on strong partnerships (SDG 17) across academia, industry, government, and NGOs, with initiatives like the tissue engineering and Regenerative Medicine International Society fostering global collaboration and knowledge exchange [81].
Other SDGs in tissue engineering
By advancing medical science and promoting sustainable practices, biomaterials and technologies in tissue engineering contribute to the broader objectives of sustainable development in various indirect ways, including SDG 1 (No Poverty), SDG 2 (Zero Hunger), SDG 6 (Clean Water and Sanitation), SDG 7 (Affordable and Clean Energy), SDG 13 (Climate Action), SDG 14 (Life Below Water), SDG 15 (Life on Land), and SDG 16 (Peace, Justice, and Strong Institutions). For instance, sustainable practices in the production and disposal of biomaterials and tissue engineering products help minimize water usage, pollution including micro-plastics, and overall environmental impact. The development of sustainable biomaterials and tissue engineering technologies with low carbon footprints contributes to climate change mitigation. Biomaterials derived from marine organisms, such as chitosan from crustacean shells, are used in tissue engineering applications, supporting sustainable resource utilization and reducing waste [82]. These practices help protect marine ecosystems and promote the sustainable use of ocean resources. Tissue engineering technologies promote the sustainable use of terrestrial ecosystems; for instance, silk fibroin from silk cocoons can be used in applications such as tissue scaffolds for regenerative medicine, contributing to the conservation of biodiversity and the sustainable use of land-based resources [80]. Lastly, by ensuring that advanced medical treatments are accessible and affordable to all, including marginalized and low-income populations, tissue engineering promotes social equity and justice.
Challenges and future outlook
The future direction of tissue engineering is poised to be defined by its capability to integrate both technological advancements and sustainable practices, which is especially critical in the realm of UN SDGs. Tissue engineering has historically focused on three core elements viz. cell-based, growth factor-based, and scaffold-based approaches. However, with increasing awareness of environmental impacts and medical innovation, future trends must address both functional medical requirements and sustainability goals.
However, implementing sustainability principles in tissue engineering to comply with UN SDGs faces several challenges. For instance, sourcing eco-friendly and sustainable biomaterials that maintain quality and biocompatibility is challenging, as many traditional materials are derived from non-renewable resources or involve energy-intensive processes. Next, sustainable practices, including using green materials and processes, often have higher initial costs, making it difficult for tissue engineering solutions to be economically competitive. Next, techniques like 3D printing, scaffold fabrication, and sterilization processes are energy-intensive, posing challenges in reducing the carbon footprint without compromising the quality of engineered tissues. Next, developing effective waste management strategies for bio-based and synthetic materials, including disposal of laboratory waste and chemical residues, is a challenge. Next, scaling up sustainable tissue engineering processes while ensuring reproducibility and standardization can be complex, particularly when using diverse and innovative materials. Next, meeting both sustainability standards and regulatory requirements for clinical use is demanding, as guidelines for eco-friendly practices in the biomedical sector are still evolving. Next, conducting comprehensive life cycle assessment to evaluate the environmental impact of tissue-engineered products throughout their lifespan is challenging due to the complexity of manufacturing processes and the lack of standardized metrics. Next, sustainability in tissue engineering requires collaboration between biologists, engineers, environmental scientists, and economists, which can be challenging to coordinate effectively. Further, there is lack of awareness and training on sustainability practices among researchers, manufacturers, and healthcare professionals within the tissue engineering field. Lastly, convincing stakeholders, including clinicians, industry partners, and the public, to adopt sustainable practices is challenging.
Yet, these challenges in implementing sustainability in tissue engineering present several opportunities and a positive future outlook. First, advancing bio-based polymers, recycled materials, and upcycled biowaste offers eco-friendly alternatives without compromising biocompatibility. Next, automated fabrication, 3D bioprinting, and scalable bioreactor systems can reduce costs, making sustainable products more economically viable. Next, integrating renewable energy and low-energy techniques can significantly reduce the carbon footprint of tissue-engineered products. Next, biodegradable scaffolds, closed-loop systems, and chemical recycling can enhance waste management, leading to sustainable laboratory practices. Next, establishing clearer guidelines and international standards for sustainable tissue engineering will facilitate compliance and clinical translation. Next, robust life cycle assessment tools tailored for biomedical products will help optimize processes and minimize environmental impact. Next, increased collaboration among diverse experts can drive innovations balancing sustainability and biomedical efficacy. Next, expanding training and educational programs will create a new generation of researchers skilled in sustainable practices. Next, rising demand for eco-friendly medical products can drive industry investments in sustainability and create market advantages. Lastly, emphasizing reuse, recycling, and upcycling of materials aligns tissue engineering with circular economy principles, reducing waste and resource consumption.
Summary
In summary, tissue engineering has evolved to incorporate a wide range of biomaterials such as polymers, metals, ceramics, composites, and decellularized materials. These materials are engineered to mimic the ECM, providing structural and functional support for cell growth and tissue regeneration. Technologies such as bioprinting, electrospinning, decellularization, cell sheet engineering, and microfluidics have further enhanced the precision and efficiency of creating complex tissue constructs. The integration of these technologies with sustainable practices pave the way for environmentally friendly and ethically responsible medical solutions. The alignment of tissue engineering with SDG 3 is evident through the development of advanced medical treatments that improve health outcomes and accessibility. Additionally, the field's contributions to SDGs 4, 5, 8, 9, 10, 11, 12 and 17 highlight its broader impact on social and economic development. Furthermore, tissue engineering indirectly supports SDGs 1, 2, 6, 7, 13, 14, 15 and 16 by promoting sustainable practices, reducing environmental impact, and fostering inclusive opportunities. As tissue engineering continues to evolve, the emphasis on affordability and accessibility, especially in low-resource settings, will ensure that the field not only meets medical needs but also fosters social equity. Overall, tissue engineering represents a transformative domain that can achieve sustainable healthcare solutions, advancing both human health and environmental stewardship.
Data availability
No datasets were generated or analysed during the current study.
References
https://sdgs.un.org/goals, (n.d.). https://sdgs.un.org/goals.
Langer R, Vacanti JP. Tissue engineering. Science. 1993;260:920–6. https://doiorg.publicaciones.saludcastillayleon.es/10.1126/science.8493529.
Vacanti CA. The history of tissue engineering. J Cell Mol Med. 2006;10:569–76. https://doiorg.publicaciones.saludcastillayleon.es/10.1111/j.1582-4934.2006.tb00421.x.
Vacanti CA, Vacanti JP. Functional organ replacement, the new technology of tissue engineering. Surg Technol Int. 1991;1:43–9.
O’Connell CD, Duchi S, Onofrillo C, Caballero-Aguilar LM, Trengove A, Doyle SE, Zywicki WJ, Pirogova E, Di Bella C. Within or without you? A perspective comparing in situ and ex situ tissue engineering strategies for articular cartilage repair. Adv Healthc Mater. 2022;11:2201305. https://doiorg.publicaciones.saludcastillayleon.es/10.1002/adhm.202201305.
Jaklenec A, Stamp A, Deweerd E, Sherwin A, Langer R. Progress in the tissue engineering and stem cell industry “are we there yet?” Tissue Eng Part B Rev. 2012;18:155–66. https://doiorg.publicaciones.saludcastillayleon.es/10.1089/ten.teb.2011.0553.
Engler AJ, Sen S, Sweeney HL, Discher DE. Matrix elasticity directs stem cell lineage specification. Cell. 2006;126:677–89. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.cell.2006.06.044.
Rouwkema J, Gibbs S, Lutolf MP, Martin I, Vunjak-Novakovic G, Malda J. In vitro platforms for tissue engineering: implications for basic research and clinical translation. J Tissue Eng Regen Med. 2011;5:e164–7. https://doiorg.publicaciones.saludcastillayleon.es/10.1002/term.414.
Chang H-I, Wang Y. Cell Responses to Surface and Architecture of Tissue Engineering Scaffolds, in: D. Eberli (Ed.), Regen. Med. Tissue Eng. - Cells Biomater., InTech, 2011. https://doiorg.publicaciones.saludcastillayleon.es/10.5772/21983.
Howard D, Buttery LD, Shakesheff KM, Roberts SJ. Tissue engineering: strategies, stem cells and scaffolds. J Anat. 2008;213:66–72. https://doiorg.publicaciones.saludcastillayleon.es/10.1111/j.1469-7580.2008.00878.x.
Jorgensen AM, Mahajan N, Atala A, Murphy SV. Advances in skin tissue engineering and regenerative medicine. J Burn Care Res. 2023;44:S33–41. https://doiorg.publicaciones.saludcastillayleon.es/10.1093/jbcr/irac126.
Jaiswal C, Chandra V, Pant KK. skin tissue engineering: a review. J Adv Sci Res. 2022;13:01–11. https://doiorg.publicaciones.saludcastillayleon.es/10.55218/JASR.202213401.
Gayanthry G, Athira RK, Anju MS, PR AK, PR HV, Kasoju N, Komath M. Mesenchymal stem cell culture in aligned porous hydroxyapatite scaffolds using a multiwell plate bioreactor for bone tissue engineering. MedComm - Future Med. 2022;1:e17. https://doiorg.publicaciones.saludcastillayleon.es/10.1002/mef2.17.
Ansari M. Bone tissue regeneration: biology, strategies and interface studies. Prog Biomater. 2019;8:223–37. https://doiorg.publicaciones.saludcastillayleon.es/10.1007/s40204-019-00125-z.
Ye KY, Black LD. Strategies for tissue engineering cardiac constructs to affect functional repair following myocardial infarction. J Cardiovasc Transl Res. 2011;4:575. https://doiorg.publicaciones.saludcastillayleon.es/10.1007/s12265-011-9303-1.
Chiu LLY. Cardiac tissue engineering: current state and perspectives. Front Biosci. 2012;17:1533. https://doiorg.publicaciones.saludcastillayleon.es/10.2741/4002.
Ming Z, Tang X, Liu J, Ruan B. Advancements in research on constructing physiological and pathological liver models and their applications utilizing bioprinting technology. Molecules. 2023;28:3683. https://doiorg.publicaciones.saludcastillayleon.es/10.3390/molecules28093683.
Yi S, Xu L, Gu X. Scaffolds for peripheral nerve repair and reconstruction. Exp Neurol. 2019;319:112761. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.expneurol.2018.05.016.
Beena M, Ameer JM, Kasoju N. Optically clear silk fibroin films with tunable properties for potential corneal tissue engineering applications: a process–property–function relationship study. ACS Omega. 2022;7:29634–46. https://doiorg.publicaciones.saludcastillayleon.es/10.1021/acsomega.2c01579.
Xue J, Feng B, Zheng R, Lu Y, Zhou G, Liu W, Cao Y, Zhang Y, Zhang WJ. Engineering ear-shaped cartilage using electrospun fibrous membranes of gelatin/polycaprolactone. Biomaterials. 2013;34:2624–31. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.biomaterials.2012.12.011.
Hamilton NJI, Birchall MA. Tissue-engineered larynx: future applications in laryngeal cancer. Curr Otorhinolaryngol Rep. 2017;5:42–8. https://doiorg.publicaciones.saludcastillayleon.es/10.1007/s40136-017-0144-6.
Demarco FF, Conde MCM, Cavalcanti BN, Casagrande L, Sakai VT, Nör JE. Dental pulp tissue engineering. Braz Dent J. 2011;22:3–13. https://doiorg.publicaciones.saludcastillayleon.es/10.1590/S0103-64402011000100001.
Lee EJ, Kasper FK, Mikos AG. Biomaterials for tissue engineering. Ann Biomed Eng. 2014;42:323–37. https://doiorg.publicaciones.saludcastillayleon.es/10.1007/s10439-013-0859-6.
Abbott RD, Kaplan DL. Engineering biomaterials for enhanced tissue regeneration. Curr Stem Cell Rep. 2016;2:140–6. https://doiorg.publicaciones.saludcastillayleon.es/10.1007/s40778-016-0039-3.
Keane TJ, Badylak SF. Biomaterials for tissue engineering applications. Semin Pediatr Surg. 2014;23:112–8. https://doiorg.publicaciones.saludcastillayleon.es/10.1053/j.sempedsurg.2014.06.010.
Navarro M, Michiardi A, Castaño O, Planell JA. Biomaterials in orthopaedics. J R Soc Interface. 2008;5:1137–58. https://doiorg.publicaciones.saludcastillayleon.es/10.1098/rsif.2008.0151.
Hu H, Xu F-J. Rational design and latest advances of polysaccharide-based hydrogels for wound healing. Biomater Sci. 2020;8:2084–101. https://doiorg.publicaciones.saludcastillayleon.es/10.1039/D0BM00055H.
Fu L-H, Qi C, Ma M-G, Wan P. Multifunctional cellulose-based hydrogels for biomedical applications. J Mater Chem B. 2019;7:1541–62. https://doiorg.publicaciones.saludcastillayleon.es/10.1039/C8TB02331J.
Arif ZU, Khalid MY, Sheikh MF, Zolfagharian A, Bodaghi M. Biopolymeric sustainable materials and their emerging applications. J Environ Chem Eng. 2022;10:108159. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.jece.2022.108159.
Beena Unni A, Muringayij Joseph T. Enhancing polymer sustainability: eco-conscious strategies. Polymers. 2024;16:1769. https://doiorg.publicaciones.saludcastillayleon.es/10.3390/polym16131769.
Arif ZU, Khalid MY, Noroozi R, Hossain M, Shi HH, Tariq A, Ramakrishna S, Umer R. Additive manufacturing of sustainable biomaterials for biomedical applications. Asian J Pharm Sci. 2023;18:100812. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.ajps.2023.100812.
Khalid MY, Arif ZU, Al Rashid A, Bukhari SM, Hossain M, Koç M. Shape-memory and self-healing properties of sustainable cellulosic nanofibers-based hybrid materials for novel applications. Giant. 2024;19:100299. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.giant.2024.100299.
Qian H, Liu J, Wang X, Pei W, Fu C, Ma M, Huang C. The state-of-the-art application of functional bacterial cellulose-based materials in biomedical fields. Carbohydr Polym. 2023;300:120252. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.carbpol.2022.120252.
Eldeeb AE, Salah S, Elkasabgy NA. Biomaterials for tissue engineering applications and current updates in the field: a comprehensive review. AAPS PharmSciTech. 2022;23:267. https://doiorg.publicaciones.saludcastillayleon.es/10.1208/s12249-022-02419-1.
Khang G, Lee SJ, Kim MS, Lee HB. Biomaterials: Tissue Engineering and Scaffolds, in: J.G. Webster (Ed.), Encycl. Med. Devices Instrum., 1st ed., Wiley, 2006. https://doiorg.publicaciones.saludcastillayleon.es/10.1002/0471732877.emd029.
Kim HS, Kumbar SG, Nukavarapu SP. Biomaterial-directed cell behavior for tissue engineering. Curr Opin Biomed Eng. 2021;17:100260. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.cobme.2020.100260.
Mobasseri R, Tian L, Soleimani M, Ramakrishna S, Naderi-Manesh H. Bio-active molecules modified surfaces enhanced mesenchymal stem cell adhesion and proliferation. Biochem Biophys Res Commun. 2017;483:312–7. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.bbrc.2016.12.146.
Umuhoza D, Yang F, Long D, Hao Z, Dai J, Zhao A. Strategies for tuning the biodegradation of silk fibroin-based materials for tissue engineering applications. ACS Biomater Sci Eng. 2020;6:1290–310. https://doiorg.publicaciones.saludcastillayleon.es/10.1021/acsbiomaterials.9b01781.
Nava MM, Raimondi MT, Pietrabissa R. Controlling self-renewal and differentiation of stem cells via mechanical cues. J Biomed Biotechnol. 2012;2012:1–12. https://doiorg.publicaciones.saludcastillayleon.es/10.1155/2012/797410.
Chen C, Bang S, Cho Y, Lee S, Lee I, Zhang S, Noh I. Research trends in biomimetic medical materials for tissue engineering: 3D bioprinting, surface modification, nano/micro-technology and clinical aspects in tissue engineering of cartilage and bone. Biomater Res. 2016;20:10. https://doiorg.publicaciones.saludcastillayleon.es/10.1186/s40824-016-0057-3.
Arif ZU, The role of polysaccharide-based biodegradable soft polymers in the healthcare sector, Adv. Ind. Eng. Polym. Res. 2024;S2542504824000241. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.aiepr.2024.05.001.
Anupama Sekar J, Athira RK, Lakshmi TS, Velayudhan S, Bhatt A, Anil Kumar PR, Kasoju N. 3D Bioprinting in Tissue Engineering and Regenerative Medicine: Current Landscape and Future Prospects, in: B. Bhaskar, P. Sreenivasa Rao, N. Kasoju, V. Nagarjuna, R.R. Baadhe (Eds.), Biomater. Tissue Eng. Regen. Med., Springer Singapore, Singapore, 2021: pp. 561–580. https://doiorg.publicaciones.saludcastillayleon.es/10.1007/978-981-16-0002-9_17.
Gong P, Zheng W, Xiao D, Jiang X. Microscale methods to assemble mammalian cells into tissue-like structures. Sci China Life Sci. 2012;55:862–71. https://doiorg.publicaciones.saludcastillayleon.es/10.1007/s11427-012-4385-9.
Kasoju N, Ye H, Cui Z, Ramakrishna S. Electrospinning and electrospraying in biomedical engineering, in: Biomed Appl Electrospinning Electrospraying, Elsevier, 2021: pp. 375–393. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/B978-0-12-822476-2.00015-7.
Hou Q, Grijpma DW, Feijen J. Preparation of interconnected highly porous polymeric structures by a replication and freeze-drying process. J Biomed Mater Res B Appl Biomater. 2003;67B:732–40. https://doiorg.publicaciones.saludcastillayleon.es/10.1002/jbm.b.10066.
Rowley AT, Nagalla RR, Wang S, Liu WF. Extracellular matrix-based strategies for immunomodulatory biomaterials engineering. Adv Healthc Mater. 2019;8:1801578. https://doiorg.publicaciones.saludcastillayleon.es/10.1002/adhm.201801578.
Bružauskaitė I, Bironaitė D, Bagdonas E, Bernotienė E. Scaffolds and cells for tissue regeneration: different scaffold pore sizes—different cell effects. Cytotechnology. 2016;68:355–69. https://doiorg.publicaciones.saludcastillayleon.es/10.1007/s10616-015-9895-4.
Leipzig ND, Shoichet MS. The effect of substrate stiffness on adult neural stem cell behavior. Biomaterials. 2009;30:6867–78. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.biomaterials.2009.09.002.
J.H. Lee, J. Kisiday, A.J. Grodzinsky, Tissue‐Engineered Versus Native Cartilage: Linkage between Cellular Mechano‐Transduction and Biomechanical Properties, in: G. Bock, J. Goode (Eds.), Novartis Found. Symp., 1st ed., Wiley, 2003: pp. 52–69. https://doiorg.publicaciones.saludcastillayleon.es/10.1002/0470867973.ch5.
Singhal AR, Agrawal CM, Athanasiou KA. Salient degradation features of a 50:50 PLA/PGA scaffold for tissue engineering. Tissue Eng. 1996;2:197–207. https://doiorg.publicaciones.saludcastillayleon.es/10.1089/ten.1996.2.197.
Bacakova L, Filova E, Parizek M, Ruml T, Svorcik V. Modulation of cell adhesion, proliferation and differentiation on materials designed for body implants. Biotechnol Adv. 2011;29:739–67. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.biotechadv.2011.06.004.
Murugan R, Ramakrishna S. Nano-featured scaffolds for tissue engineering: a review of spinning methodologies. Tissue Eng. 2006;12:435–47. https://doiorg.publicaciones.saludcastillayleon.es/10.1089/ten.2006.12.435.
Ng R, Zang R, Yang KK, Liu N, Yang S-T. Three-dimensional fibrous scaffolds with microstructures and nanotextures for tissue engineering. RSC Adv. 2012;2:10110. https://doiorg.publicaciones.saludcastillayleon.es/10.1039/c2ra21085a.
Leong K, Chua C, Sudarmadji N, Yeong W. Engineering functionally graded tissue engineering scaffolds. J Mech Behav Biomed Mater. 2008;1:140–52. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.jmbbm.2007.11.002.
Tan B, Gan S, Wang X, Liu W, Li X. Applications of 3D bioprinting in tissue engineering: advantages, deficiencies, improvements, and future perspectives. J Mater Chem B. 2021;9:5385–413. https://doiorg.publicaciones.saludcastillayleon.es/10.1039/D1TB00172H.
Xie X, Chen Y, Wang X, Xu X, Shen Y, Khan AUR, Aldalbahi A, Fetz AE, Bowlin GL, El-Newehy M, Mo X. Electrospinning nanofiber scaffolds for soft and hard tissue regeneration. J Mater Sci Technol. 2020;59:243–61. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.jmst.2020.04.037.
Bahrami S, Baheiraei N, Najafi-Ashtiani M, Nour S, Razavi M, Microfluidic devices in tissue engineering, in: Biomed. Appl. Microfluid. Devices, Elsevier, 2021: pp. 209–233. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/B978-0-12-818791-3.00008-5.
Zhang Y, Organoids As a Tool to Fuel Basic Medical Research. J Complement Med Altern Healthc 2023;11. https://doiorg.publicaciones.saludcastillayleon.es/10.19080/JCMAH.2023.11.555823.
Hunt NC, Lako M. Tissue engineering using pluripotent stem cells: multidisciplinary approaches to accelerate bench-to-bedside transition. Regen Med. 2016;11:495–8. https://doiorg.publicaciones.saludcastillayleon.es/10.2217/rme-2016-0095.
Fu R-H, Wang Y-C, Liu S-P, Shih T-R, Lin H-L, Chen Y-M, Sung J-H, Lu C-H, Wei J-R, Wang Z-W, Huang S-J, Tsai C-H, Shyu W-C, Lin S-Z. Decellularization and recellularization technologies in tissue engineering. Cell Transpl. 2014;23:621–30. https://doiorg.publicaciones.saludcastillayleon.es/10.3727/096368914X678382.
Elzinga FA, Khalili B, Touw DJ, Prins JR, Olinga P, Leuvenink HGD, van Goor H, Gordijn SJ, Nagelkerke A, Mian P. Placenta-on-a-chip as an in vitro approach to evaluate the physiological and structural characteristics of the human placental barrier upon drug exposure: a systematic review. J Clin Med. 2023;12:4315. https://doiorg.publicaciones.saludcastillayleon.es/10.3390/jcm12134315.
Gargus ES, Rogers HB, McKinnon KE, Edmonds ME, Woodruff TK. Engineered reproductive tissues. Nat Biomed Eng. 2020;4:381–93. https://doiorg.publicaciones.saludcastillayleon.es/10.1038/s41551-020-0525-x.
Fogg K, Tseng N-H, Peyton SR, Holeman P, Mc Loughlin S, Fisher JP, Sutton A, Shikanov A, Gnecco JS, Knight KM, Slaby EM, Weaver JD, Hashemi NN, Zhang Y, House MD, Vogt BJ, Aguado BA, Bradford JC, Robinson JL, Thomas PK, Lau AG, Oyen ML. Roadmap on biomaterials for women’s health. J Phys Mater. 2023;6:012501. https://doiorg.publicaciones.saludcastillayleon.es/10.1088/2515-7639/ac90ee.
Blum KM, Mirhaidari GJM, Breuer CK. Tissue engineering: Relevance to neonatal congenital heart disease. Semin Fetal Neonatal Med. 2022;27:101225. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.siny.2021.101225.
Dellacherie MO, Li A, Lu BY, Verbeke CS, Gu L, Stafford AG, Doherty EJ, Mooney DJ. Single-shot mesoporous silica rods scaffold for induction of humoral responses against small antigens. Adv Funct Mater. 2020;30:2002448. https://doiorg.publicaciones.saludcastillayleon.es/10.1002/adfm.202002448.
Zarubova J, Zhang X, Hoffman T, Hasani-Sadrabadi MM, Li S. Biomaterial-based immunoengineering to fight COVID-19 and infectious diseases. Matter. 2021;4:1528–54. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.matt.2021.02.025.
Dogan A, Eser Elcin A, Murat EY. Translational applications of tissue engineering in cardiovascular medicine. Curr Pharm Des. 2017;23:903–14. https://doiorg.publicaciones.saludcastillayleon.es/10.2174/1381612823666161111141954.
Waksman R. The disappearing stent: when plastic replaces metal. Circulation. 2012;125:2291–4. https://doiorg.publicaciones.saludcastillayleon.es/10.1161/CIRCULATIONAHA.112.103911.
Neves LS, Rodrigues MT, Reis RL, Gomes ME. Current approaches and future perspectives on strategies for the development of personalized tissue engineering therapies. Expert Rev Precis Med Drug Dev. 2016;1:93–108. https://doiorg.publicaciones.saludcastillayleon.es/10.1080/23808993.2016.1140004.
Desai N, Alex A, AbdelHafez F, Calabro A, Goldfarb J, Fleischman A, Falcone T. Three-dimensional in vitro follicle growth: overview of culture models, biomaterials, design parameters and future directions. Reprod Biol Endocrinol. 2010;8:119. https://doiorg.publicaciones.saludcastillayleon.es/10.1186/1477-7827-8-119.
Wang X, Wu D, Li W, Yang L. Emerging biomaterials for reproductive medicine. Eng Regen. 2021;2:230–45. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.engreg.2021.11.006.
Mukherjee S, Darzi S, Paul K, Werkmeister JA, Gargett CE. Mesenchymal stem cell-based bioengineered constructs: foreign body response, cross-talk with macrophages and impact of biomaterial design strategies for pelvic floor disorders. Interface Focus. 2019;9:20180089. https://doiorg.publicaciones.saludcastillayleon.es/10.1098/rsfs.2018.0089.
Colazo JM, Evans BC, Farinas AF, Al-Kassis S, Duvall CL, Thayer WP. Applied bioengineering in tissue reconstruction, replacement, and regeneration. Tissue Eng Part B Rev. 2019;25:259–90. https://doiorg.publicaciones.saludcastillayleon.es/10.1089/ten.teb.2018.0325.
Nichols JE, Niles JA, Vega SP, Argueta LB, Eastaway A, Cortiella J. Modeling the lung: Design and development of tissue engineered macro- and micro-physiologic lung models for research use. Exp Biol Med. 2014;239:1135–69. https://doiorg.publicaciones.saludcastillayleon.es/10.1177/1535370214536679.
Maughan E, Lesage F, Butler CR, Hynds RE, Hewitt R, Janes SM, Deprest JA, Coppi PD. Airway tissue engineering for congenital laryngotracheal disease. Semin Pediatr Surg. 2016;25:186–90. https://doiorg.publicaciones.saludcastillayleon.es/10.1053/j.sempedsurg.2016.02.012.
Ali ASM, Berg J, Roehrs V, Wu D, Hackethal J, Braeuning A, Woelken L, Rauh C, Kurreck J. Xeno-Free 3D bioprinted liver model for hepatotoxicity assessment. Int J Mol Sci. 2024;25:1811. https://doiorg.publicaciones.saludcastillayleon.es/10.3390/ijms25031811.
Singh G, Mohapatra M. Three-dimensional printing, bioink, organ printing, and tissue engineering technologies, and their application in modern anatomical pedagogy. Natl J Clin Anat. 2023;12:223–6. https://doiorg.publicaciones.saludcastillayleon.es/10.4103/NJCA.NJCA_182_23.
Ashammakhi N, GhavamiNejad A, Tutar R, Fricker A, Roy I, Chatzistavrou X, Hoque Apu E, Nguyen K-L, Ahsan T, Pountos I, Caterson EJ. Highlights on advancing frontiers in tissue engineering. Tissue Eng Part B Rev. 2022;28:633–64. https://doiorg.publicaciones.saludcastillayleon.es/10.1089/ten.teb.2021.0012.
Díaz Lantada A, De Maria C. Sustainable open-source medical devices manufactured with green biomaterials and accessible resources. Curr Opin Biomed Eng. 2023;28:100500. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.cobme.2023.100500.
Kasoju N, Bora U. Silk fibroin in tissue engineering. Adv Healthc Mater. 2012;1:393–412. https://doiorg.publicaciones.saludcastillayleon.es/10.1002/adhm.201200097.
Bertram TA, Johnson PC, Tawil BJ, Van Dyke M, Hellman KB. Enhancing tissue engineering and regenerative medicine product commercialization: the role of science in regulatory decision-making for the TE/RM product development. Tissue Eng Part A. 2015;21:2476–9. https://doiorg.publicaciones.saludcastillayleon.es/10.1089/ten.tea.2015.0136.
Omoregie IP, Osagie AD, Ogochukwu OO. Crustacean nanochitosan-based bioremediation of nanoplastic-polluted aquatic habitat: a review pursuant to SDG 6. Sci Afr. 2023;21:e01881. https://doiorg.publicaciones.saludcastillayleon.es/10.1016/j.sciaf.2023.e01881.
Acknowledgements
Authors acknowledge the support from SCTIMST Trivandrum and Department of Science and Technology (GOI).
Funding
Department of Science and Technology, Ministry of Science and Technology, Government of India through Technical Research Centre for Biomedical Devices (TRC-P8311).
Author information
Authors and Affiliations
Contributions
NK - conceptualization, formal analysis, writing - review and editing, visualization, funding acquisition, project administration, resources, supervision. AS – methodology, data curation, writing - original draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable, as it does not involve the use of any animal or human data or tissue.
Consent for publication
Not applicable, as it does not contain any individual person’s data in any form.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kasoju, N., Sunilkumar, A. Convergence of tissue engineering and sustainable development goals. Biotechnol Sustain Mater 1, 20 (2024). https://doiorg.publicaciones.saludcastillayleon.es/10.1186/s44316-024-00021-y
Received:
Accepted:
Published:
DOI: https://doiorg.publicaciones.saludcastillayleon.es/10.1186/s44316-024-00021-y